
Understanding Anhedonia
Anhedonia, a term often encountered in mental health discussions and relatively unknown to most lay-people, particularly in relation to depression. Anhedonia signifies a diminished capacity to experience pleasure. The term itself is derived from the Greek words “an-“, meaning without, and “hedone”, meaning pleasure, effectively describing a lack of pleasure or joy. Theodule Ribot, a French Psychologist, first coined the term in the 1800s. Recognized in the DSM-5 as a key symptom of major depressive disorder and other mental health conditions, it manifests as a notable lack of interest and a reduced ability to feel pleasure in activities that were previously enjoyable.
The Clinical Perspective
Clinically, anhedonia is not considered a separate diagnosis but plays a significant role in the diagnosis and treatment of depressive disorders. It’s often seen as a reduction in the intensity of feelings, especially those associated with pleasure and enjoyment.
Symptoms of Anhedonia
Individuals with anhedonia may display a range of symptoms, including:
- Loss of Interest: A significant drop in interest or pleasure in all or almost all daily activities.
- Reduced Emotional Responsiveness: A lack of reactivity to typically pleasurable stimuli, including diminished emotional responses to positive events.
- Social Withdrawal: Avoiding social gatherings and activities that were previously engaging.
- Lack of Motivation: Difficulty starting or completing activities due to a belief that they won’t be enjoyable.
- Flat Affect: Showing little facial expression or having a blunted emotional affect.
- Changes in Appetite and Sleep Patterns: These can include decreased appetite or overeating, insomnia, or oversleeping.
- Difficulty in Experiencing Intimacy and Affection: Challenges in feeling or expressing love and affection towards others.
- Cognitive Impairments: Problems with concentration, decision-making, and memory can be linked to anhedonia.
The Impact on Daily Life
Anhedonia can deeply affect daily life, influencing hobbies, social interactions, and overall satisfaction. It can lead to social isolation and impair relationships, reducing personal fulfillment.
Biological and Psychological Factors have been Linked to the brain’s reward pathways, particularly involving dopamine, anhedonia can arise from stress, trauma, or emotional burnout, leading to emotional numbness.
Coping with Anhedonia
Addressing anhedonia may involve therapy, possibly medication, and lifestyle changes that modify exercise, diet, and mindfulness practices. Gradually reengaging in activities, even if not immediately pleasurable, can be beneficial in overcoming anhedonia.
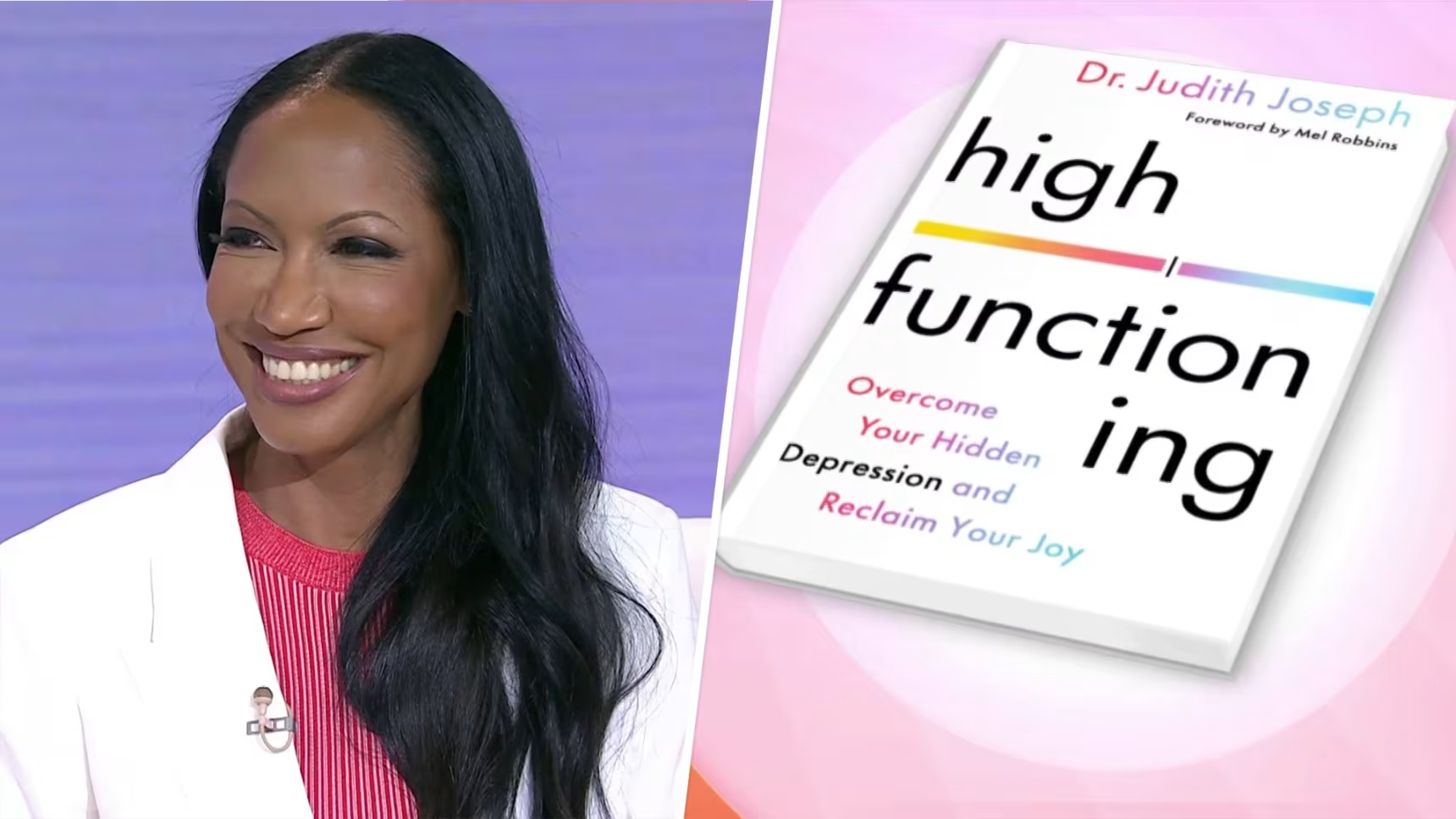
Dr. Judith’s Insight
Dr. Judith emphasizes the importance of understanding anhedonia in mental health. She advocates for comprehensive treatment approaches that address both biological and psychosocial elements. Much of the anhedonia literature looks at substance abuse and anhedonia and Dr. Judith believes that there may be overlap in those with HFD as well as other postpandemic phenomena where individuals are escaping in excessive behaviors (excessive shopping, excessive online or social media use, excessive work, etc) to cope with unprocessed trauma.
Exploring Anhedonia Further
For those looking to understand their experiences with anhedonia, Dr. Judith provides a quiz as a self-reflection tool. It is not part of a formal study nor is it a part of a formal diagnosis but instead it may serve as a resource for personal insights. You may want to consider visiting the website to take the quiz and discuss the findings with your licensed medical provider as this is not a formal diagnosis that can be made without the patient/provider relationship. Visit Dr. Judith’s Anhedonia Quiz for more insights and to participate in this valuable self-assessment.
Disclaimer: You may want to consider your individual mental health needs with a licensed medical professional. This page is not medical advice.

Dr. Judith Joseph, a board-certified Psychiatrist and Media Consultant with over 1 million followers on social media, leads the First-of-its-kind study on High-Functioning Depression. While there is a multitude of research on depression and dysthymia, there is very little on depression in the prodromal phase in people who have symptoms of depression but do not meet criteria for a major depressive episode because they are functioning at a high capacity and they do not report or acknowledge being in significant distress. These individuals do not necessarily identify with the emotion “depression” until someone points out that they are exhibiting symptoms of depression and or anhedonia. While High Functioning Depression is a term that has risen recently in the past 5 years in the online discourse and mental health circles, it is not yet recognized amongst medical professionals and is not in the diagnostic manual for psychiatry (DMS-5). Many individuals during and after the Covid-19 pandemic began to present to Dr. Judith’s practice using the term, “High Functioning Depression” and there have been reports of HFD worsening without treatment into fatal forms of mental illnesses. This along with Dr. Judith’s online followers asking for more resources on HFD, led to Dr. Judith and her research team submitting the first of its kind High Functioning Depression study to the IRB in 2023. She is currently enrolling individuals into this study to learn more about the risk factors and unique presentations of individuals who identify as having High Functioning Depression. Dr. Judith holds degrees in biology, chemistry, religion medicine, and business from prestigious institutions such as Duke University and Columbia, and has post-doctoral and research training at Columbia University and NYU. Passionate about inclusive mental health treatments, Dr. Judith heads a dedicated team of 10 women focused on innovative research for various mental health conditions. Her lab pioneers high-functioning conditions research, develops psychometric scales for mood and anxiety, and promotes evidence-based approaches. Her lab has enrolled patients into phase 2-4 clinical research studies aiding in the development of novel treatments for pediatric, adult and geriatric conditions ranging from ADHD to Alzheimer’s dementia. Some of the novel treatments have become FDA approve and now help to treat millions of people worldwide. Her clinical research site, Manhattan Behavioral Medicine has participated in both Pharma and NIH funded research and is one of the few clinical research sites solely owned and solely operated by a black woman Principal Investigator. This is important as it is well known that for many years minority populations and women were largely underrepresented in clinical research. Dr. Judith is dedicated to creating space for diversity and inclusion in this space so that research and evidence-based treatments are representative of all populations. Dr. Judith Joseph is committed to advancing mental health treatment and embracing diversity in her work.